Causes of Merkel cell carcinoma
Jump to Section:
What causes Merkel cell carcinoma?
Causes and Risks at a Glance
Merkel cell carcinoma Merkel cell carcinoma A skin cancer composed of cells that look microscopically similar to normal Merkel cells present in the skin. MCC was first described in 1972 and only in the 1990s was the CK20 antibody developed to make it easily identifiable by pathologists. Many doctors and patients are not aware of this cancer because of its recent description and relative rarity (~2,000 cases/year in the US--roughly 30 times less common than melanoma). About 40% of patients treated for MCC will experience a recurrence, making it far more aggressive than most other types of skin cancer, including melanoma. (MCC) is caused by the Merkel cell Merkel cell Merkel cells are found in the lower part of the epidermis. Although the exact function of Merkel cells is unknown, they are thought to be touch receptors. Also known as neuroendocrine cells, they have machinery similar to nerve cells and to hormone-secreting (endocrine) cells. polyomavirus or by extensive exposure to ultraviolet radiation (sunlight). Groups who are at higher risk for MCC include men, people with light-colored skin, people with weakened immune systems, and people over 60 years of age.
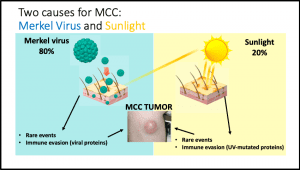
Merkel Cell Polyomavirus causes the majority of Merkel cell carcinoma cases in the USA and most countries.
In 2008, scientists discovered a virus present in MCC tumors which they named Merkel cell polyomavirus (Merkel virus). They found that in 8 of the 10 MCC tumors they studied, the DNA of this virus had been inserted into the DNA of the MCC tumor cells. Importantly, they also found evidence that the virus had inserted its DNA before the infected cell began rapidly dividing to form the tumor. This led them to think that Merkel virus was a contributing factor in the development of MCC tumors 1. Since this discovery, many additional studies have verified their findings 2. Scientists are now beginning to understand the mechanisms underlying virus-driven MCC, also called “virus-positive MCC”.
A Closer Look
Most people have been infected with Merkel virus at some point in their lives and will never show any symptoms of infection. We now know that in the vast majority of Merkel virus infections, the viral DNA does not integrate with the DNA of the infected cell 3. Studies show that when the viral DNA combines with the host cell DNA, it changes the way that the genetic instructions of the virus are read so that modified viral proteins are formed. These proteins can make the infected cells divide more quickly, which is an early step in the formation of a tumor 3. Scientists are still exploring why the viral DNA sometimes integrates with the DNA of the infected cell while it usually does not. One idea is that high levels of ultraviolet radiation from the sun can lead to certain changes in the DNA of the virus which allow the viral DNA to integrate 4.
Exposure to sunlight is involved in virus-positive and virus-negative MCC.
There is substantial evidence that ultraviolet (UV) radiation from the sun contributes to the development of MCC. Studies show that MCC is most commonly found on sun-exposed areas of the body, such as the head, neck, and arms. MCC cases are more common in very sunny areas compared to areas with less sun 3. Additionally, MCC is more likely to be found on the left side of the face or the left arm, which are the areas that are most exposed to the sun while driving 5. MCC is also much more common in people with light-colored skin, which is more easily damaged by UV rays than more pigmented skin, as well as in people over age 60, who have more cumulative UV exposure over their lifetimes than younger people 6.
In MCC tumors where the Merkel virus is not detected (virus-negative MCC), UV exposure is thought to initiate tumor development by causing many small changes in the DNA of skin cells that accumulate over time. These changes can eventually cause cells to grow and divide more quickly than healthy cells, which is an early step in the development of a tumor 7.
UV exposure may also contribute to virus-positive MCC. UV radiation is thought to cause changes in the Merkel virus which allow the virus to integrate its DNA with that of the infected cell 3. This integration of viral and host cell DNA starts a process which can eventually cause MCC to develop. A study also showed that exposure to UV radiation increased the levels of a MCPyV protein that is known to contribute to the development of MCC tumors 8.
Who is most likely to get Merkel cell carcinoma?
Men are at higher risk for MCC.
In a group of over 14,000 MCC patients, 62% were men and 38% were women 6. Scientists are not sure why MCC is more common in men, but studies in mice may provide some clues. Male mice show more damage after exposure to UV radiation than female mice 9 and have lower levels of antioxidant enzymes, which can prevent damage to DNA after UV exposure 10. Additional studies suggest that estrogen, a hormone which is higher in women than in men, may play a protective role against UV damage and the development of tumors in the skin 11.
Most MCC patients have light-colored skin.
Over 96.4% of MCC patients are white 6. This is likely due to increased susceptibility to UV damage in skin with minimal pigmentation.
A weakened immune system predisposes to MCC.
People with weakened immune systems are at higher risk of developing MCC and make up about 9% of all MCC patients in the United States 12. These patients can include people with diseases such as chronic lymphocytic leukemia chronic lymphocytic leukemia A slow-growing type of leukemia (white blood cell cancer) associated with immune suppression. Patients with CLL have a markedly increased risk and severity of Merkel cell carcinoma. 13 or HIV 14, which impair the function of immune cells, and people who get treatments to suppress their immune systems, such as kidney or heart transplant recipients 15 or people with autoimmune disease 16.
The immune system plays an important role in controlling MCC. Some patients with strong immune systems are able to eliminate their first MCC tumor without realizing it, and do not notice their MCC until it has appeared for a second time, typically in a lymph node lymph node A rounded mass of lymphatic tissue that is usually surrounded by connective tissue and about the size of a green pea. Lymph nodes filter lymphatic fluid, also know as lymph, which is fluid that drains from the tissues of the body and contains immune cells. Cancer cells often travel through lymph vessels and lodge and grow in lymph nodes, sometimes causing the nodes to markedly increase in size. . These patients are referred to as patients with an “unknown primary tumor” and they tend to do better compared to patients who develop MCC in a lymph node and still have a primary tumor in their skin 17. Several studies also show that patients with more immune cells present in their tumor have improved survival 18,.
Based on these observations, scientists are investigating ways to boost the immune response against MCC tumors. Click here to learn more about clinical trials that aim to boost the patient immune response to MCC. Meanwhile, it is sensible for patients to eat well, exercise, manage their stress, and get plenty of sleep in order to promote good immune health.
Most MCC patients are over age 60.
The risk of developing MCC increases markedly with advancing age. In the United States, 88% of MCC patients are over the age of 60 years at time of diagnosis and the average age of MCC patients at diagnosis is around 76 years old 6. Older people may be at higher risk of MCC because their skin has been exposed to the sun for a long time and because the immune system becomes less robust with advanced age.
Footnotes
- 1Feng H, Shuda M, Chang Y, et al. Clonal integration of a polyoma virus in human Merkel cell carcinoma. Science 2008; 319:1096–100.
- 2Moshiri AS, Doumani R, Yelistratova L, et al. Polyomavirus-negative Merkel cell carcinoma: a more aggressive subtype based on analysis of 282 cases using multimodal tumor virus detection. Investig. Dermatol., 137 (2017), pp. 819-827.
- 3Becker JC, Stang A, DeCaprio JA, et al. Merkel cell carcinoma. Nat Rev Dis Primers. 2017; 3: 17077.
- 4Church CD and Nghiem P. How does the Merkel polyomavirus lead to a lethal cancer? Many answers, many questions, and a new mouse model. J Inves Dermatol. 2015; 135: 1221-1224.
- 5Paulson KG, Iyer JG, and Nghiem P. Asymmetrical lateral distribution of melanoma and Merkel cell carcinoma in the United States. Journal of AAD. 2011; 65(1): 35-39.
- 6Harms KL, Healy MA, Nghiem P, et al. Analysis of prognostic factors from 9387 Merkel cell carcinoma cases forms the basis for the new 8th edition AJCC staging system. Ann Surg Oncol. 2016; 23(11): 3564–3571.
- 7Wong SQ, Waldeck K, Vergara IA, et al. UV-Associated mutations underlie the etiology of MCV-negative Merkel cell carcinomas. Cancer Res. 2015; 75(24): 5228-34.
- 8Mogha A, Fautrel A, Mouthcet N, et al. Merkel cell polyomavirus small T antigen mRNA level is increased following in vivo UV-radiation. PLoS One. 2010; 5(7): e11423.
- 9Thomas-Ahner JM, Wulff BC, Tober KL, et al. Gender differences in UVB-induced skin carcinogenesis, inflammation, and DNA damage. Cancer Res. 2007; 67: 3468-74.
- 10Tomas-Zapico C, Alvarez-Garcia O, Sierra V, et al. Oxidative damage in the livers of senescence-accelerated mice: a gender-related response. Can J Physiol Pharmacol. 2006; 84: 213-220.
- 11Vina J, Sastre J, Pallardo FV, et al. Modulation of longevity-associated genes by estrogens or phytoestrogens. Biol Chem. 2008; 389: 273-277.
- 12KG Paulson, JG Iyer, A Blom. Systemic immune suppression as a stage-independent predictor of diminished Merkel cell carcinoma-specific survival. J Invest Dermatol. 2013; 133(3): 642-646.
- 13Tadmor T, Liphshitz I, Aviv A, et al. Increased incidence of chronic lymphocytic leukaemia and lymphomas in patients with Merkel cell carcinoma – a population based study of 335 cases with neuroendocrine skin tumour. 2012; 157(4): 457-462.
- 14Engels EA, Frisch M, Goedart JJ, et al. Merkel cell carcinoma and HIV infections. Lancet. 2002; 359(9305): 497-498.
- 15Penn I & First MR. Merkel’s cell carcinoma in organ recipients: report of 41 cases. Transplantation. 1999; 68(11): 1717-21.
- 16Hemminki K, Liu X, Ji J, et al. Kaposi sarcoma and Merkel cell carcinoma after autoimmune disease. Int J Cancer. 2012; 131(3) E326-328.
- 17Merkel cell carcinoma patients presenting without a primary lesion have elevated markers of immunity, higher tumor mutation burden and improved survival. Clin Cancer Res. 2017; 24(4): 963-971.
- 18Feldmeyer L, Hudgens CW, Ray-Lyons G, et al. Density, distribution, and composition of immune infiltrates correlate with survival in Merkel cell carcinoma. Clinical cancer research. 2016; 22(22): 5553-63.
- 19Paulson KG, Iyer JG, Simonson WT, et al. CD8+ lymphocyte intratumoral infiltration as a stage-independent predictor of Merkel cell carcinoma survival: a population-based study. Am. J. Clin. Pathol. 2014; 142(4): 452-458.
- 20Sihto H, Bohling T, Kavola H, et al. Tumor infiltrating immune cells and outcome of Merkel cell carcinoma: a population-based study. Cancer Res. 2012; 18(10): 2872-81.