
Radiation therapy
Jump to Section:
Purpose of radiation therapy
Radiation therapy Radiation therapy The use of radiation to kill cancer cells and shrink tumors. Merkel cell carcinoma is a highly radiation sensitive cancer in most cases. , also referred to as radiotherapy or XRT, is the treatment of cancer cancer A term used to describe diseases in which abnormal cells continually divide without normal regulation. Cancerous cells may invade surrounding tissues and may spread to other regions of the body via blood and the lymphatic system. with penetrating beams of energy waves or streams of particles that can destroy cancer cells. Radiation therapy is delivered to the cancer cells and a margin margin The edge or perimeter of the tissue removed in cancer surgery. The margin is described as "clear" or "negative" when the pathologist sees no sign of cancer cells under the microscope, suggesting that all of the cancer has been removed. The margin is described as "positive" or "involved" when the pathologist finds cancer cells in the edge of the tissue. This suggests that not all of the cancer has been removed. Certain cancers such as Merkel cell carcinoma can have negative microscopic margins despite residual cancer cells being left behind because MCC often "skips" via local lymphatics to adjacent areas and does not grow a single continuous mass. of surrounding apparently normal tissue, referred to as the radiation field. Radiation therapy damages the genetic material of cancer cells making them unable to grow. Radiation therapy also damages healthy cells in the field of radiation.
“Adjuvant” radiation therapy is radiotherapy that is used to destroy any cancer cells that may remain after surgery has removed all of the tumor that is visible.
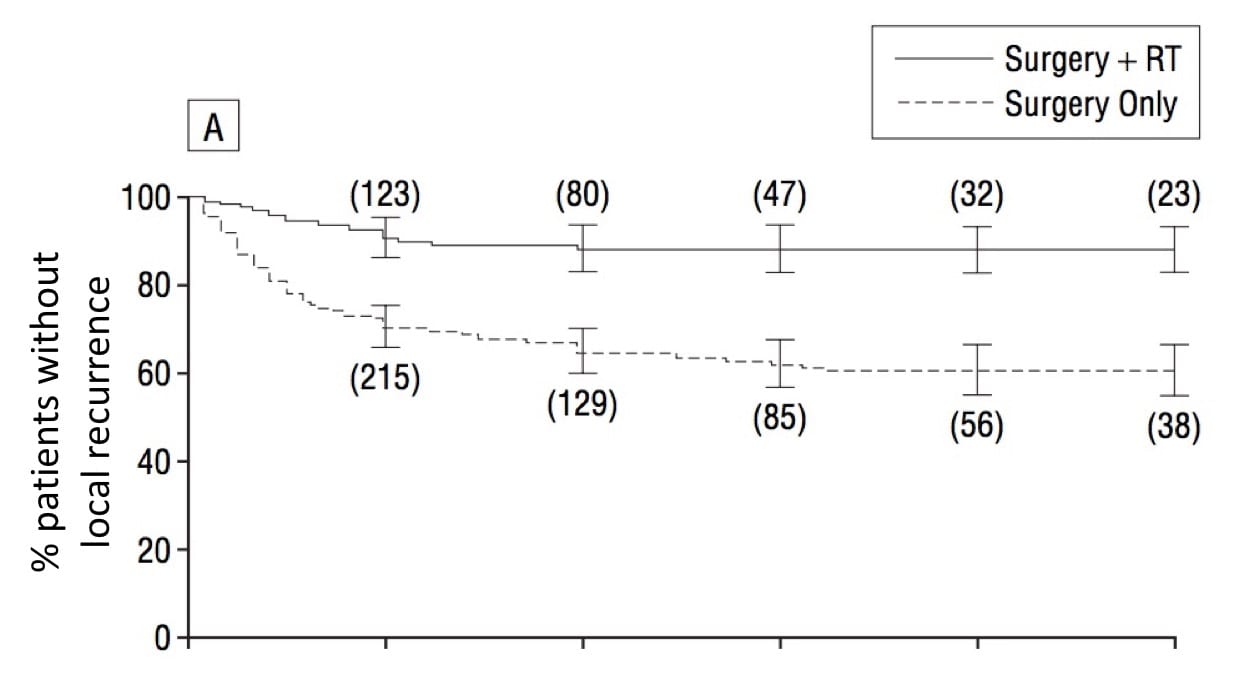
An analysis of the available literature and our experience caring for MCC patients since 1999 shows that adding radiotherapy to surgery is associated with a statistically significant decrease in local local Affecting only the site of origin, without evidence of spreading. Compare to systemic. and nodal recurrence. Some studies also suggest that adding radiation to surgery may improve a patient’s chance of survival, but this is more controversial.1 Where wide excision excision The removal of tissue of interest by surgery. is not possible, radiotherapy is sometimes given alone and has an excellent ability to control the tumor. These data suggest a role for radiotherapy for many patients with stage stage Physicians determine the stage of cancer by performing physical exams and tests. Stages describe the extent of cancer within the body, especially whether the disease has spread (metastasized) from the primary site to other parts of the body. I, II & III disease.
A Closer Look
The dose of radiotherapy is measured in units called Gray (Gy). The total dose of radiation therapy should typically be greater than or equal to 50 Gy. Radiation therapy is usually administered in a doctor’s office in small doses for 10-15 minutes, 5 days a week (e.g., Monday through Friday) over a set number of weeks (most commonly for 5 weeks).
Who this works for
Radiation therapy can markedly lower the risk of MCC recurrence in the irradiated areas ( primary site primary site The area of the body where the abnormal tissue first appeared. and or draining lymph node draining lymph node The particular lymph node(s) to which the lymph fluid from an area of tissue flows. basin). We usually recommend patients receive radiation if they have a significant risk of local-nodal recurrence (typically >15%), are generally healthy, want to maximize the chance of not having the cancer come back in the areas at risk, and can travel daily to a local radiation therapy facility for the 5-6 week treatment period.
A new approach we are taking with some patients is to deliver a single dose (8 Gy) of radiation to decrease the chance that the primary tumor will recur. We are currently studying outcomes in these patients but it is clear that side effects are much lower while effectiveness appears to be similar to traditional adjuvant radiation therapy given over many weeks.
Who this doesn’t work for
Patients who have very low risk disease, as defined by having all six of the favorable features below, are not likely to benefit from adjuvant radiation therapy.
We are currently not routinely recommending radiation therapy for such low-risk cases. The six favorable features include:
- Primary tumor ≤1 cm in largest dimension
- Negative sentinel lymph node biopsy sentinel lymph node biopsy Removal and examination of the "sentinel" lymph node(s). Sentinel nodes are the first lymph nodes to which cancer cells spread from a primary lesion. To identify the sentinel lymph node(s), a radioactive substance and/or dye is injected near the primary lesion. The surgeon uses a Geiger counter to find the lymph node(s) containing the radioactive substance or looks for the lymph node(s) stained by the dye. The surgeon then removes the sentinel lymph node(s) and sends them to a pathologist to check for the presence of cancer.
- No chronic immune suppression (HIV disease, leukemia/lymphoma, transplant of heart or kidney or liver)
- No lympho-vascular invasion in the primary tumor ( pathologist pathologist A doctor who specializes in identifying diseases by examining cells and tissues under a microscope. may need to be asked to go back to the original biopsy biopsy The removal of cells or tissue in order to determine the presence, characteristics, or extent of a disease by a pathologist usually using microscopic analysis. and specifically comment on this feature’s presence or absence).
- Confidently negative microscopic margins after excision
- Primary tumor not located on the head or neck (sites that are associated with a higher risk of recurrence).
Side effects
Common side-effects of radiation therapy in the area being treated include loss of hair, skin irritation (like a sunburn), and changes in the color and texture of the skin. Radiation to the adjacent lymph nodes may cause swelling of the arm or leg. Such swelling may be long-lasting and is more likely if surgery has also been carried out in the same nodal area. A frequent side effect is fatigue, which usually resolves within a month or two after the radiotherapy is stopped. Accordingly, it is important to eat a well-balanced diet and get plenty of rest. A radiation oncologist radiation oncologist A doctor who specializes in using radiation to treat cancer. X-rays ("photons") are used to penetrate more deeply and "electron" beam therapy is used to target more superficial cancer sites. may adjust the dose or schedule of radiation therapy based on the side effects. Localized radiation therapy typically does not lead to nausea, vomiting, or hair loss outside of the irradiated area.
Often used in conjunction with
Surgery and/or systemic systemic Affecting the entire body. Compare to local. therapy
FAQs
Do I need radiation?
Radiation is one type of treatment used in some cancers. Radiation Oncologists plan and administer this type of treatment. Radiation therapy is often an important part of treatment for MCC. Usually radiation is given to the primary site (on the skin) of the tumor. If the sentinel lymph node biopsy was positive, radiation is often indicated to those lymph nodes.
What is the best way to decide if an MCC patient should have radiation?
While there is agreement that radiation therapy lowers the risk of MCC recurrence, there is great controversy as to exactly which patients should receive this therapy. The side effects, cost, and inconvenience of radiation therapy can be significant. Patients with extremely low risk disease should not receive radiation, and patients with high risk disease should be offered this therapy. Determining which moderate-risk disease patients should receive radiation is very tricky and needs to be customized for each patient’s philosophy regarding recurrence risk versus side effects. Ideally, this discussion should take place with a multi-disciplinary team that is very familiar with the relevant literature and the risks and benefits of radiation therapy for MCC.
What is single-fraction radiation for MCC?
In some cases, especially if MCC has spread beyond the local-nodal area, we have successfully used a single, larger dose (8 Gy) of radiation to shrink and sometimes eliminate a given metastatic lesion. This approach has relatively few side effects and may work nicely together with systemic immune stimulation therapy. We described this approach in a 2015 report on 93 tumors treated in 26 patients.
Should all patients participate in complementary or alternative therapies for their cancer?
No. Participation in these ‘scientifically unproven’ approaches to cancer therapy should be strictly voluntary. Some patients are very keen to use these approaches and others have no interest. We never push our patients to engage in any specific alternative approach.
Understand the Science
The following clinical publications and scientific research provide additional in-depth information about radiation therapy.