Causes of Merkel cell carcinoma
Jump to Section:
Overview of Merkel cell carcinoma causes
Factors strongly associated with the development of MCC include age over 65 years, fair skin, history of extensive sun exposure, chronic immune suppression (e.g., kidney or heart transplantation or HIV), and the Merkel cell Merkel cell Merkel cells are found in the lower part of the epidermis. Although the exact function of Merkel cells is unknown, they are thought to be touch receptors. Also known as neuroendocrine cells, they have machinery similar to nerve cells and to hormone-secreting (endocrine) cells. polyomavirus.
Risk factors for Merkel cell carcinoma
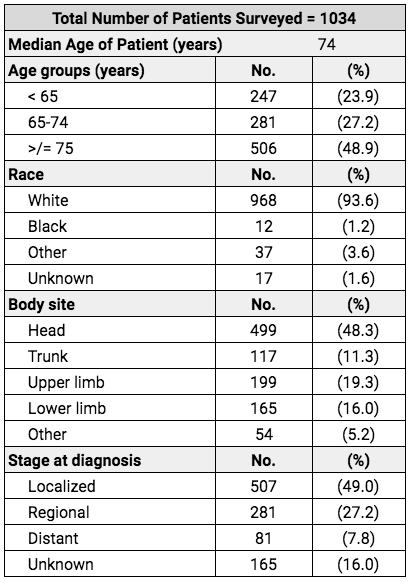
Extensive information on characteristics of patients with MCC comes from a study of 1,034 patients summarized in the table below.1 The average (median) age of the patients with MCC was 74 years. The most common sites of involvement were head followed by arms (upper limb). At the time of diagnosis, half of the patients had disease that was only present in the skin, while the other half had MCC that was already present in lymph nodes or distant sites.
Age & Merkel cell carcinoma
The risk of developing MCC increases with advancing age. 75% of MCC patients are over the age of 65 years at time of diagnosis, with the average age for developing MCC being 74. MCC is slightly more common in men than women for each age group (see graph below).
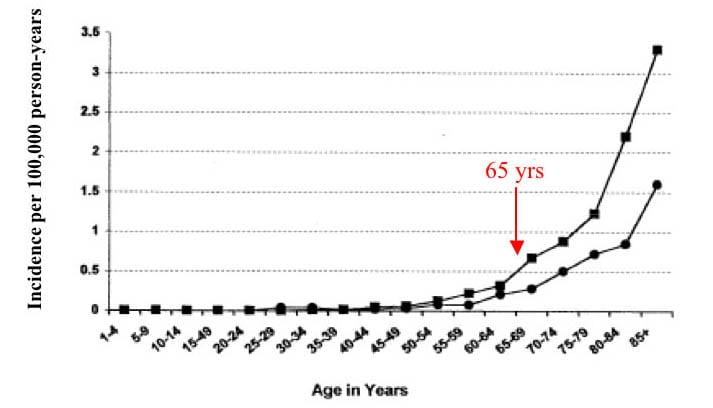
Frequency of MCC by age & sex: men (square) & women (circle). Adapted from Agelli, 2003.
Sunlight & Merkel cell carcinoma
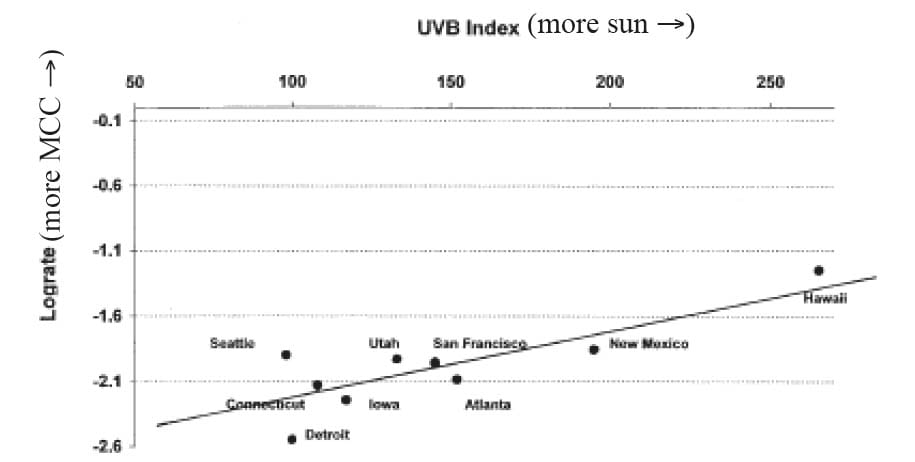
It is believed that ultraviolet radiation from the sun plays a significant role in the development of MCC. MCC is most commonly found on sun-exposed areas of the body (e.g., head, neck, arms) in older Caucasian individuals, who may also have other sun-induced skin cancers. There are more MCC cases in sunny climates (Hawaii) as opposed to areas with less sun (Connecticut) (see graph below). While extensive sun exposure is a risk factor for MCC, MCC can also occur on sun-protected skin, such as a hair-covered scalp.
Immune function & Merkel cell carcinoma
Patients with weakened immune systems are at significantly higher risk of developing MCC. Conditions associated with weakened immunity include HIV/AIDS, kidney or heart transplantation, and autoimmune diseases requiring medications that suppress the immune system, chronic lymphocytic leukemia chronic lymphocytic leukemia A slow-growing type of leukemia (white blood cell cancer) associated with immune suppression. Patients with CLL have a markedly increased risk and severity of Merkel cell carcinoma. (CLL) and certain types of lymphoma. The risk of developing MCC is 8 times greater in HIV patients, 10 times greater in organ transplant patients, and about 40 times greater in CLL.2 3 4 Long-term suppression of the immune system (for many years) appears to be a risk factor for MCC in some patients. While patients with profound immune suppression are at a higher risk of developing MCC, over 90% of all people who develop MCC have no known immune deficiency.3
The immune system is also very important after diagnosis of MCC. Patients whose tumors show a robust immune response with certain immune cells present in their tumor (killer T cells) tend to do better.5 MCC patients without a primary tumor (no original skin lesion lesion An area of abnormal tissue that may be either benign or malignant. ) also do better, likely because their immune system was able to eliminate the primary tumor and thus are more likely to be able to fight small amounts of MCC elsewhere in the body as well.6 In contrast, patients on medications that reduce immune function are at higher risk of having their MCC recur.
Researchers are currently investigating ways to help boost the immune response to MCC tumor (see Clinical Trials). Meanwhile, it is sensible to eat well, exercise, and get plenty of sleep to promote good immune health. Although not proven in humans, some complementary medical approaches aim to improve immune function.
The Merkel cell polyomavirus (MCPyV)
In 2008, the Merkel cell polyomavirus (MCPyV) was discovered by the University of Pittsburgh laboratory of Drs Patrick Moore & Yuan Chang and found to be frequently present in MCC tumors.7 The virus was found in 8 of 10 tumors tested, and was associated with the DNA of the tumor cells in such a way to suggest that it is involved in the development of MCC. Since then, many studies have validated this initial report, finding MCPyV in the vast majority (about 80%) of MCC patients.8 9 Studies now show that the majority of people have been exposed to MCPyV by adulthood, but it appears that the virus does not cause any symptoms except in the very rare situations in which it leads to MCC (Nicol 2013, others).
A Closer Look
Antibodies to the outer “shell” of the virus (called the capsid protein) are found in 90% of MCC patients and 60% of those without MCC.10 MCC patients whose immune systems have been exposed to the virus and produce the antibodies to the capsid protein tend to fight MCC more effectively than patients whose bodies do not produce the VP1 antibody. This observation further supports the importance of the immune system in fighting this cancer.
FAQs
What causes MCC?
Recent genetic studies have shown that Merkel cell carcinomas are caused either by mutations induced by sunlight or by the Merkel cell polyomavirus. Risk factors strongly associated with the development of MCC include fair skin, a history of extensive sun exposure, chronic immune suppression (kidney or heart transplantation or HIV), and over age 50.
Who gets MCC?
Individuals over the age of 65 are far more likely to develop MCC. Fair skin and a history of extensive sun exposure also increase the chances. MCC is associated with weakened immune function, such as in patients with HIV or organ transplants. However, over 90% of people who get MCC have no known immune suppression.
Footnotes
- 1Agelli M, Clegg LX. Epidemiology of primary Merkel cell carcinoma in the United States [published correction appears in J Am Acad Dermatol. 2004 May;50(5):733]. J Am Acad Dermatol. 2003;49(5):832-841. doi:10.1016/s0190-9622(03)02108-x
- 2Penn I, First MR. Merkel’s cell carcinoma in organ recipients: report of 41 cases. Transplantation. 1999;68(11):1717-1721. doi:10.1097/00007890-199912150-00015
- 3Heath M, Jaimes N, Lemos B, et al. Clinical characteristics of Merkel cell carcinoma at diagnosis in 195 patients: the AEIOU features. J Am Acad Dermatol. 2008;58(3):375-381. doi:10.1016/j.jaad.2007.11.020
- 4Engels EA, Frisch M, Goedert JJ, Biggar RJ, Miller RW. Merkel cell carcinoma and HIV infection. Lancet. 2002;359(9305):497-498. doi:10.1016/S0140-6736(02)07668-7
- 5Iyer JG, Storer BE, Paulson KG, et al. Relationships among primary tumor size, number of involved nodes, and survival for 8044 cases of Merkel cell carcinoma. J Am Acad Dermatol. 2014;70(4):637-643. doi:10.1016/j.jaad.2013.11.031
- 6Deneve JL, Messina JL, Marzban SS, et al. Merkel cell carcinoma of unknown primary origin. Ann Surg Oncol. 2012;19(7):2360-2366. doi:10.1245/s10434-011-2213-2
- 7Feng H, Shuda M, Chang Y, Moore PS. Clonal integration of a polyomavirus in human Merkel cell carcinoma. Science. 2008;319(5866):1096-1100. doi:10.1126/science.1152586
- 8Becker JC, Kauczok CS, Ugurel S, Eib S, Bröcker EB, Houben R. Merkel cell carcinoma: molecular pathogenesis, clinical features and therapy. J Dtsch Dermatol Ges. 2008;6(9):709-719. doi:10.1111/j.1610-0387.2008.06830.x
- 9Rodig SJ, Cheng J, Wardzala J, et al. Improved detection suggests all Merkel cell carcinomas harbor Merkel polyomavirus. J Clin Invest. 2012;122(12):4645-4653. doi:10.1172/JCI64116
- 10Carter JJ, Paulson KG, Wipf GC, et al. Association of Merkel cell polyomavirus-specific antibodies with Merkel cell carcinoma. J Natl Cancer Inst. 2009;101(21):1510-1522. doi:10.1093/jnci/djp332
Clinical Publications
The following clinical publications and scientific research provide additional in-depth information about causes of merkel cell carcinoma.